In this post, we share insights from patient conversations on the diagnosis and treatment journey of Dermatomyositis – a widespread skin condition affecting numerous individuals across the globe. It is estimated that there are just under 3,000 new cases of Dermatomyositis in the United States each year.
For those who are eager to contribute to the advancement of Dermatomyositis research, we invite you to explore our research registry here!
How is Dermatomyositis diagnosed?
Diagnosing Dermatomyositis involves a series of tests and evaluations to identify its presence and severity. Some tests that may be used to diagnose Dermatomyositis include blood tests, EMG, MRI, and muscle/skin biopsy.
For a diagnosis of Dermatomyositis, a patient may have one of the following symptoms on their skin:
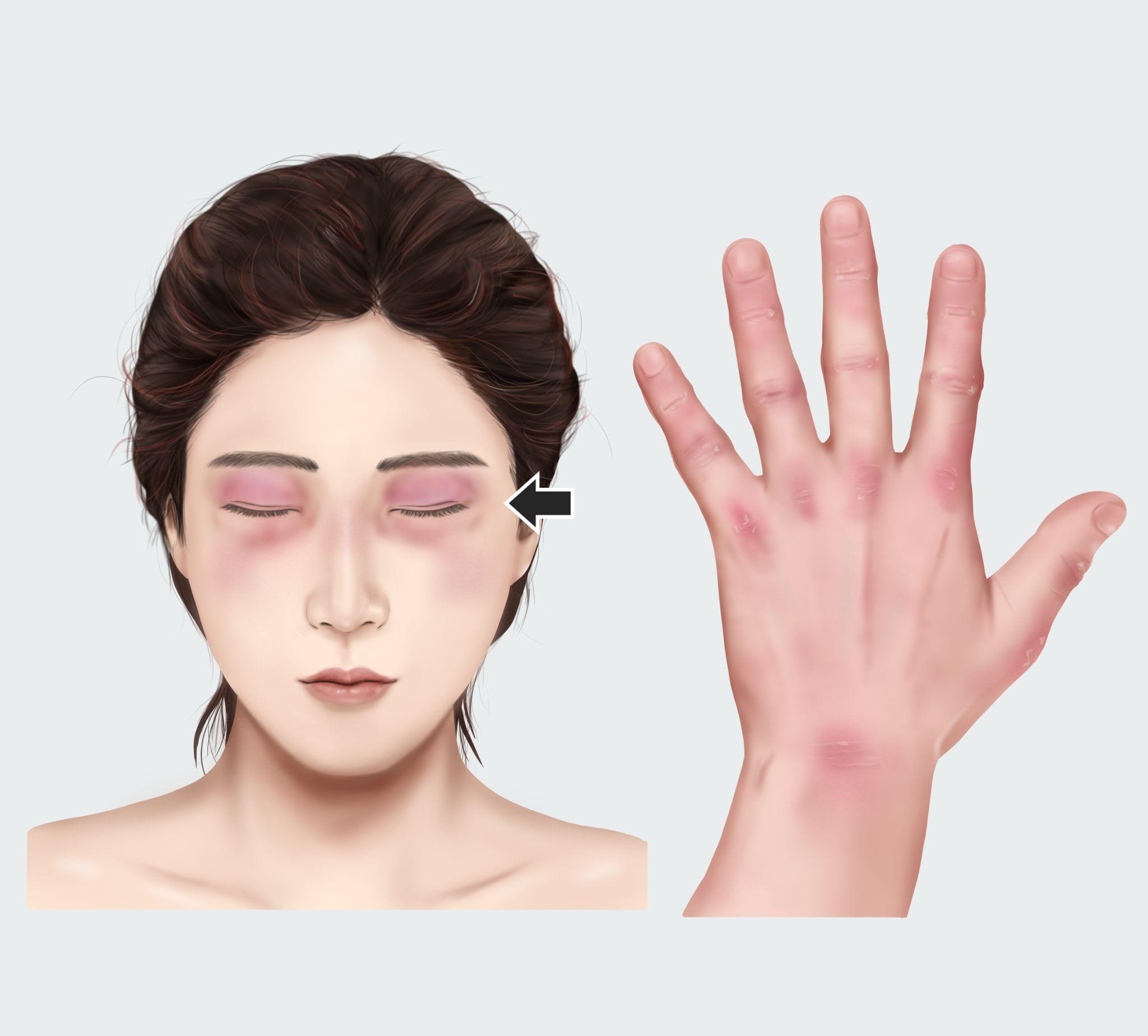
- Heliotrope Rash – a red or purple rash that occurs on or around the eyelids.
- Periungual Telangiectasias – also known as “spider veins”, are broken blood vessels that occur near the surface of the skin.
- Gottron’s Papules – small bumps that are either red or purple in color, and that occur on the knuckles and the joints of the fingers.
- Shawl or “V” sign – a red rash that tends to be shaped in a “shawl” pattern over the shoulders, arms, and upper back, and also in a V-shape pattern over the front of the neck and chest.
- A skin biopsy that shows signs of Dermatomyositis – Along with one of these symptoms of the skin, other criteria are looked for including signs of systemic inflammation, arthritis, fever, muscle pain, trouble talking or swallowing, and other possible indicators of the condition.
For more detailed information about how Dermatomyositis is diagnosed, The Myositis Association is a great resource.
The symptoms of Dermatomyositis can be uncomfortable and difficult to live with. One patient spoke with us about the physical strain of their symptoms, saying, “Living with Dermatomyositis has been tough. I can’t wear my favorite clothes, and even simple tasks are a struggle.”
Existing treatments can help to alleviate some of the symptoms of Dermatomyositis, and further research may yield more hope and comfort for patients suffering from this condition.
Who treats Dermatomyositis? And how is it treated?
The most common doctors to treat Dermatomyositis are rheumatologists. Dermatologists and neuromuscular experts also frequently assist with diagnosis. There is currently no cure for the condition, but some existing treatment methods include physical therapy, anti-inflammatory medications, immunosuppressive drugs, immunoglobulin, and surgery.
Even with existing treatments, patients still sometimes struggle to find solutions for managing their Dermatomyositis symptoms. On the topic of clinical research as a treatment option, one patient shared with Leapcure, “My disease is flaring up but I can’t afford the treatment. I tried insurance and applying for charity but nothing has worked out and my only hope is potentially participating in clinical research.”
Through research, other treatment options are being explored that give patients suffering from Dermatomyositis new optimism. One patient said about their experience participating in clinical research for Dermatomyositis, “I have been living with DM for a couple of years now, but before giving up, my daughters suggested I explore clinical trials as an option. This thought gave me peace because I could help others in the future. The hope made me feel brand new again.”
To learn more about Dermatomyositis, find groups and resources, and to share more about your Dermatomyositis journey, feel free to explore our resource page here!



Leave a Reply